-
- Find Care
-
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
-
-
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
- Participate in Research
-
- Contact us
-
- For Innovators
- Commercialization Guide for Innovators
-
-
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Getting Started
- New to Mass General Brigham
- International Patient Care
- What Is Patient Gateway?
- Planning Your Visit
- Find a Doctor (opens link in new tab)
- Appointments
- Patient Resources
- Health & Wellness
- Flu, COVID-19, & RSV
- Billing & Insurance
- Financial Assistance
- Medicare and MassHealth ACOs
- Participate in Research
- Educational Resources
- Visitor Information
- Find a Location
- Shuttles
- Visitor Policies
- Find Care
-
- Overview
- Our Virtual Care Options
- Virtual Urgent Care
- Virtual Visits for Primary & Specialty Care
- Online Second Opinions
-
- Overview
- Participate in Research
-
- Overview
- About Innovation
- About
- Team
- News
- For Industry
- Venture Capital and Investments
- World Medical Innovation Forum (opens link in new tab)
- Featured Licensing Opportunities
- For Innovators
- Commercialization Guide for Innovators
- Contact us
-
- Overview
- Information for Researchers
- Compliance Office
- Research Cores
- Clinical Trials
- Advisory Services
- Featured Research
- Two Centuries of Breakthroughs
- Advances in Motion (opens link in new tab)
- Brigham on a Mission (opens link in new tab)
- Gene and Cell Therapy Institute
- Research News
- Alzheimer's Disease
- Artificial Intelligence
-
- Overview
-
- Overview
- Residency & fellowship programs
- Brigham and Women's Hospital
- Massachusetts General Hospital
- Mass Eye and Ear
- Newton-Wellesley Hospital
- Salem Hospital
- Integrated Mass General Brigham Programs
- Centers of Expertise
- Global & Community Health
- Health Policy & Management
- Healthcare Quality & Patient Safey
- Medical Education
- For trainees
- Prospective trainees
- Incoming trainees
- Current trainees
- Continuing Professional Development
Hemorrhagic Stroke Treatment

Every year, millions of people around the world die from hemorrhagic stroke. Those who survive are often left with lingering symptoms such as weakness, speech and swallowing difficulties, and even dementia.
Christopher David Anderson, MD, MSc, a Mass General Brigham neurologist, answers common questions about hemorrhagic stroke symptoms and treatment. Dr. Anderson is chief of the Stroke and Cerebrovascular Diseases Center at Brigham and Women’s Hospital.
What is a hemorrhagic stroke?
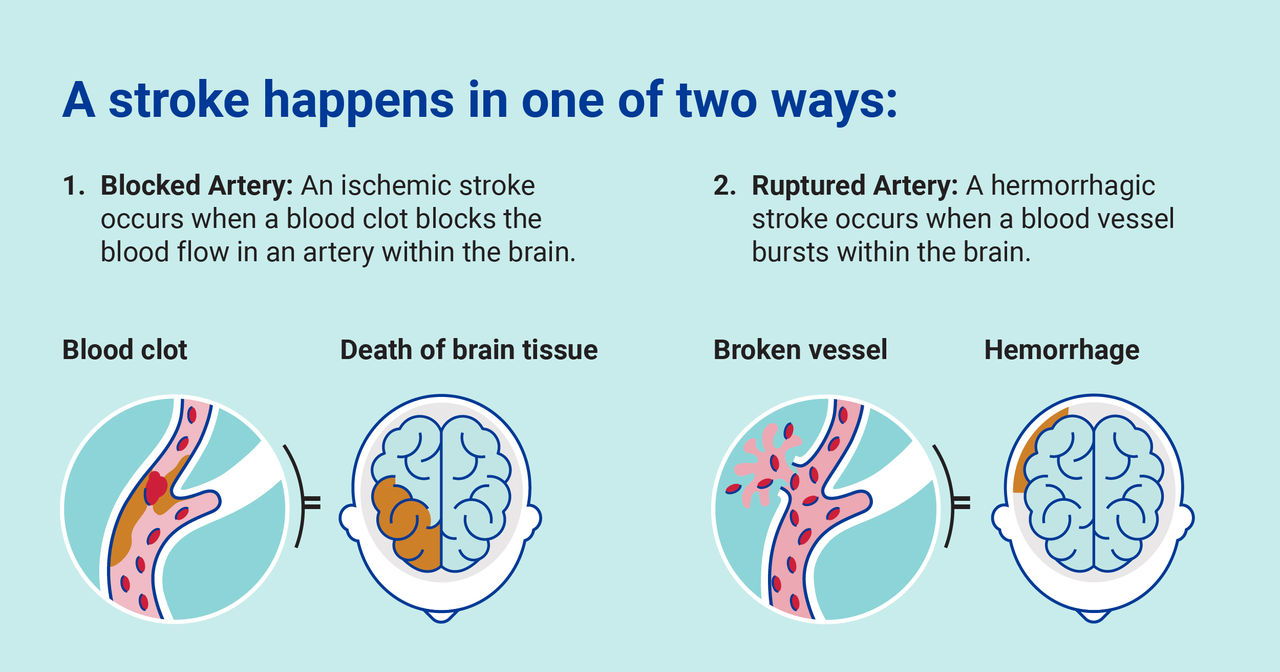
There are two kinds of strokes:
- Ischemic stroke. This is the most common type of stroke. It happens when blood clots or other particles block the blood vessels to the brain. This limits blood flow.
- Hemorrhagic stroke. “A hemorrhagic stroke is a devastating and sudden neurologic event,” explains Dr. Anderson. “It occurs when a blood vessel breaks inside the brain and causes blood to leak out, injuring the brain. The blood pushes on the brain and causes nerve cells to begin to die in just a few minutes.”
There are also two types of hemorrhagic stroke:
- Intracerebral hemorrhages bleed inside the brain.
- Subarachnoid hemorrhages bleed between the brain and the membrane that protects it.
Both are dangerous and require prompt medical care.
Why do blood vessels burst?
Blood vessels can burst for a few reasons. They may burst due to an underlying condition like an aneurysm. Sometimes, they burst because of an abnormal tangle of blood vessels called an arteriovenous malformation (AVM). Most commonly, they burst due to weakening from long-term conditions like high blood pressure.
Hemorrhagic stroke signs and symptoms
There are many potential signs and symptoms of a hemorrhagic stroke. Often, the symptoms come on fast. Warning signs include:
- Numbness or weakness in the face, arm, or leg, especially on one side of the body
- Confusion
- Inability to see out of one or both eyes, or on one side of visual space
- Trouble walking, dizziness, or loss of coordination
- A severe headache
- Seizures
- Difficulty understanding or loss of speech
- Nausea and vomiting
- Loss of alertness or consciousness
- Neck pain or stiffness and difficulty swallowing
- Abnormal tastes in the mouth
- Increased sensitivity to light
- Irregular heartbeat or breathing
What should you do if you or another person shows signs or symptoms of stroke?
When assessing stroke symptoms, remember the acronym FAST, which stands for:
- Facial drooping
- Arm weakness
- Speech difficulties
- Time
Time is critical. Act quickly if you suspect a stroke and call 911 immediately.
Every minute that passes can mean additional permanent damage to health and ability. Rarely, stroke victims may require CPR. An emergency dispatcher can coach you through the process on the phone. Note the time of symptom onset as this can be critical information for emergency responders and attending physicians.
Do not give a person with stroke symptoms any medications, including aspirin. This can potentially cause further harm, depending on the kind of stroke they are suffering. Don’t let a person with stroke symptoms drive, eat, drink, or go to sleep.
Hemorrhagic stroke treatment
There are a variety of therapies available for patients with ischemic stroke. These therapies can remove blood clots and restore blood flow.
But hemorrhagic stroke treatment options are limited.
When a patient with a hemorrhagic stroke arrives at the hospital, medical teams work to quickly lower their blood pressure. This limits further bleeding. They also work to reverse the effects of any blood-thinning medications.
If the hemorrhagic stroke is due to an aneurysm or blood vessel malformation, surgeons can often repair the blood vessel, so it doesn’t bleed again.
Today, treatment for hemorrhagic stroke is preventive. So far, there’s no treatment that can stop or reverse existing damage. But researchers are investigating ways to change that.
Risk factors for hemorrhagic stroke
High blood pressure is the biggest risk factor for hemorrhagic stroke. Researchers at Mass General Brigham are discovering new ways to identify patients who are at a high risk of developing hemorrhagic stroke or hard-to-treat blood pressure. A variety of factors, including genetics and family health history, could play a role.
There are tiny differences in our genetic code. Each one contributes slightly to our risk of many diseases, including hemorrhagic stroke.
“If we add each of those tiny risks together, we can create something called a genetic score, which collectively tells us about the risk profile for an individual patient,” explains Dr. Anderson. “This score can identify those who are at a higher risk and who might benefit specifically from preventative treatments.”
Personalized risk information means personalized treatments. In time, doctors will know how to help patients reduce their risk of hemorrhagic stroke through better control of blood pressure. And they’ll be able to identify the other unique factors that put people at risk.
